You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
In order to provide optimum treatment for cervical lesions, an interdisciplinary team must first establish a facially generated treatment plan. A crucial goal of the plan is to have the teeth dominate—but not detract from—a beautiful smile. The key to accomplishing this appearance is to create a vision of the desired outcome before beginning treatment.
Establishing the correct tooth form for the patient is based on esthetics, phonetics, and function. The critical component to the esthetic appearance of teeth is their width-to-length ratio. Three interrelated components are required to optimize tooth proportion: 1) incisal edge position; 2) tooth length; and 3) gingival level. Treatment options to position the soft-tissue level ideally include surgery and orthodontics. When performing either root-coverage grafting or esthetic crown lengthening, a determination of optimal tooth form is necessary before determining where to put the gingival level. Ideally, there should be harmony between adjacent soft-tissue levels and with the contralateral tooth. There can be slight variation, but harmony is the key element. Different surgeons and teams have varying methods for aligning the incisal edges and gingival levels. One approach is to compare the interpupillary line to the horizon, and to use one or the other as a guide for the incisal plane position and gingival level from canine to canine. Subtle variations from that relationship due to limitations imposed by function and surgery are acceptable.
Guidelines for Treating Cervical Lesions
An interdisciplinary treatment approach is the appropriate choice in cases where there is gingival recession and cervical lesions.
There are three types of cervical lesions: 1) non-carious cervical lesions (NCCLs); 2) restored cervical lesions; and 3) carious cervical lesions. Proper treatment of each of these types of cervical lesions may require placement of restorations, soft-tissue grafting, or both surgical and restorative treatment.
Treatment planning for cervical lesions is simplified by the assessment of five variables: 1) gingival dimensions; 2) depth of cervical lesion/restoration/caries; 3) depth of recession; 4) classification of recession; and 5) location of the lesion. The guidelines for treating cervical lesions based on these five variables are shown in Table 1.
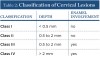
The authors have devised and published a classification of cervical lesions based on the depth of the cervical lesion and whether or not there is enamel involvement:
• Class I, shallow depth (< 0.5 mm)
• Class II, moderate depth (0.5 mm to 2 mm) with no enamel involvement
• Class III, moderate depth (0.5 mm to 2 mm) with enamel involvement
• Class IV, deep (greater than 2-mm depth) with enamel involvement (Table 2).1
The authors also subclassified cervical lesions based on the Miller classification of gingival recession present.2 Subclass A was assigned for Miller Class I or Class II recession because the root can be completely covered. Subclass B was assigned for Miller Class III and Class IV recession where the root cannot be completely covered. This classification of cervical lesions is useful for determining the appropriate treatment. Table 3 provides basic guidelines for treatment based on this classification. Generally, shallow cervical lesions should be treated with soft-tissue grafting (Figure 1 through Figure 7), deeper cervical lesions require restorative treatment, and some sites require both soft-tissue grafting and restorative treatment (Figure 8 through Figure 14).
Non-carious cervical lesions have multiple possible etiologies: 1) erosion from chemical agents; 2) abrasion from physical agents—eg, aggressive tooth brushing; and 3) abfraction from occlusal forces causing tooth flexure. Whatever the causes are, they must be managed for successful treatment.
Surgical Treatment Technique
Predictable root coverage grafting can now be accomplished with a minimally invasive surgical technique.3 This technique uses an intrasulcular approach without surface incisions for recipient site preparation, which is followed by placement of an allograft within a pouch and coronal advancement of the graft and pouch. The site preparation begins with an intrasulcular incision made with an end-cutting intrasulcular knife. This is followed by a subperiosteal blunt reflection with an Allen microsurgical elevator. The papilla is elevated from the interdental crest with a Younger-Good 7/8 curette. Root preparation with curettes and/or an ultrasonic instrument with a safe-sided diamond tip is performed after mobilization of the marginal tissue to remove shallow restorations, to eliminate any angular portions of the lesion, and to create a uniform root surface without damaging the soft tissue. Final smoothing of the root surface is accomplished with a curette. Ethylenediaminetetraacetic acid is applied to the root surface to remove the smear layer. If there is an enamel overhang coronal to the cervical lesion, it may be beveled and polished. The next step is apical extension and mobilization of the pouch by sharp dissection using a modified Orban knife. This instrument will allow dissection that is immediately supraperiosteal to ensure passive advancement of the pouch to the cementoenamel junction and to create space for the graft while maintaining an immobile recipient bed. The allograft is reconstituted, trimmed to the proper dimensions, and soaked in a platelet-rich plasma preparation for enrichment with growth factors. The graft is inserted into the pouch and aligned level with the gingival margins of the teeth, followed by coronal advancement of the graft and pouch simultaneously with a single subpapillary 6-0 polypropylene continuous sling suture. The allografts perform quite well in achieving predictable root coverage comparable to palatal connective tissue grafts when covered completely by the pouch or where graft exposure is minimal—1 mm or less.4
Typically, any gain of keratinized tissue is minimal with a submerged grafting technique as described above. Realistically, a gain of keratinized tissue is not considered to be a significant parameter for submerged grafts. While a gain of keratinized tissue is useful for assessing graft success for surface grafts such as a free gingival graft, the amount of keratinized tissue on the surface is not reflective of the gain of functional, dense collagenous connective tissue with submerged grafts. The small gain of keratinized tissue following a submerged grafting technique is not an indicator of graft success; it is related to initial graft exposure and secondary retraction of the flap’s exposure of a small portion of the graft. The advantages of this minimally invasive grafting technique include: 1) no surface incisions, thus no scarring; 2) use of an allograft eliminates need for a palatal donor site; 3) reduced patient discomfort; 4) greater acceptance of treatment; and 5) ideal esthetics. Palatal grafts are also very effective for achieving predictable root coverage, but they are subject to enlarging, thereby negatively impacting the esthetic outcome. Graft enlargement may be desirable in ridge or papilla augmentation procedures, thus palatal connective tissue may be a better choice for these applications. In sites where the graft cannot be completely covered, palatal tissue will perform better than an allograft. Otherwise, an allograft is the better choice.
Restorative Treatment Techniques
Restoration of cervical lesions should be secondary to placing the gingival level back to its ideal position. Class V restorations may be required if there is excessive depth to the lesion or significant loss of anatomic crown form.
If it is necessary to graft and restore, it is preferable to graft first because the outcome can be more precise when the restoration is placed after the root-coverage surgery. In a non-esthetic area, the restoration may be placed first while leaving the root exposed for coverage with the grafting procedure. A graft can predictably cover a root to within 3 mm of the adjacent papillae tips. If there is a difference between the mesial and distal papilla heights, the shorter of the two papillae will determine the level of root coverage. Thus, ideally, a restoration should not extend more than 3 mm apically from the papilla tip, leaving the rest of the root exposed for root-coverage grafting.5
A major challenge in restorative dentistry is restoring cervical lesions. Depending on the classification of the lesion, there may or may not be enamel involvement. In addition, the exposed dentin is sclerotic in nature, making it significantly more unpredictable to bond to than enamel or normal dentin.6 These factors will greatly impact the retention of the restoration and affect the long-term esthetic outcome due to the potential for marginal breakdown or microleakage. Class V restorations are frequently studied to determine the effectiveness of resin adhesion because of these considerations.
There are three types of cervical lesion restorations, with the predictability of the result governed by the type of bonding used in the restorative process. The critical determining factor is the extent of enamel or dentin at the margin. The first type of cervical lesion has a complete enamel border around the periphery. A one-, two-, or three-step resin-bonding system can be used in this scenario. The second type of lesion has a combination of enamel and dentin at the margin. A three-step etch-and-rinse system is recommended in this situation, as there is excellent bonding to the enamel and very good bonding to the dentin, producing an optimal long-term clinical outcome.7 A two-step self-etch adhesive system is effective; however, the disadvantage is a relatively weak bond to enamel.8 This can generally be overcome by selective etching of the enamel. With a one-bottle system that combines the primer and bonding agent together following an etch-and-rinse, there is an excellent enamel bond and a reasonable dentin bond; however, such systems are not as predictable as the three- and two-step systems.9 An all-in-one self-etch system has the poorest outcome of all the bonding systems and is not recommended.10,11 The third type of restoration involves only root structure (dentin replacement), and, therefore, has no enamel border. A glass ionomer or resin-modified glass ionomer would be an appropriate material choice.12,13 Glass ionomers offer good adhesion to dentin, fluoride release, biocompatibility, and a thermal expansion coefficient similar to natural tooth structure. If the restoration will be totally covered with gingival tissue, it should be restricted to the deepest portion of the lesion and kept as small as possible—approximately 2 mm in size. Resin-modified glass ionomers can be considered for this application.14,15 An alternative solution—if the restoration will not be covered by gingival tissue—is to use an overlay technique with resin.12 Resins are more esthetic, color-stable, finish better, and retain their surface texture and luster better than glass ionomers.
When restoring Class V lesions, tooth preparation includes roughening the surface with a diamond bur, or preferably using microabrasion with 25 μm to 50 μm aluminum oxide. Beveling of the enamel margin will improve the esthetic transition from restorative material to the tooth but does not significantly improve the retention of the restoration. Next, etching, bonding, placement of the restorative material, and curing is completed. Carbide finishing burs are used for final contouring, and then polishing is performed to achieve the appropriate surface smoothness and luster.
Conclusion
Soft-tissue grafting is an integral part of treatment of cervical lesions because of the common lack of adequate attached gingiva and root exposure associated with these lesions. Complete root coverage is a predictable outcome for Miller Class I and II recession defects, and partial root coverage can be achieved in Miller Class III defects. In the esthetic zone, it is desirable to cover as much of the root as possible, and all sites require an adequate zone of attached gingiva, especially adjacent to a restoration. Restorations are required for cervical lesions with excessive depth and significant involvement of the enamel, but they should be avoided where the lesion is shallow and the enamel involvement is minimal. Of course, some sites will require both soft-tissue grafting and placement of a restoration.
About the Authors
Edward P. Allen, DDS, PhD
Private Practice Limited to Periodontics
Dallas, Texas
Robert R. Winter, DDS
Private Practice Limited to Periodontics
Scottsdale, Arizona
References
1. Winter RR, Allen EP. Restorative and periodontal considerations for the treatment of noncarious cervical lesions. Advanced Esthetics & Interdisciplinary Dentistry. 2005;1(4):25-28.
2. Miller PD Jr. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;5(2):8-13.
3. Allen EP. Subpapillary continuous sling suturing method for soft tissue grafting with the tunneling technique. Int J Periodontics Restorative Dent. 2010;30(5):479-485.
4. Woodyard JG, Greenwell H, Hill M, et al. The clinical effect of acellular dermal matrix on gingival thickness and root coverage compared to coronally positioned flap alone. J Periodontol. 2004;75(1):44-56.
5. Allen EP, Swift EJ Jr. Crown margins in the esthetic zone. J Esthet Restor Dent. 2011;23(1):57-60.
6. Tay FR, Pashley DH. Resin bonding to cervical sclerotic dentin: a review. J Dent. 2004;32(3):173-196.
7. Van Meerbeek B, Braem M, Lanbrechts P, Vanherle G. Morphological characterization of the interface between resin and sclerotic dentin. J Dent. 1994;22(3):141-146.
8. Wilder AD Jr, Swift EJ Jr, Heymann HO, et al. A 12-year clinical evaluation of a three-step dentin adhesive in non-carious lesions. J Am Dent Assoc. 2009;140(5):526-535.
9. Swift EJ Jr. Dentin/enamel bonding. J Esthet Restor Dent. 2010; 22(6):352-353.
10. Ritter AV, Heymann HO, Swift EJ Jr, et al. Clinical evaluation of all-in-one adhesive in non-carious lesions with different degrees of dentin sclerosis. Oper Dent. 2008;33(4):370-378.
11. van Dijken JW, Pallesen U. Long-term dentin retention of etch-and-rinse and self-etch adhesives and a resin-modified glass ionomer cement in non-carious lesions. Dent Mater. 2008;24(7):915-922.
12. Francisconi LF, Scaffa PM, de Barros VR, et al. Glass ionomer cements and their role in the restoration of non-carious cervical lesions. J Appl Oral Sci. 2009:17(5):364-369.
13. van Dijken JW. Retention of a resin-modified glass ionomer adhesive in non-carious cervical lesions: A 6-year follow-up. J Dent. 2005;33(7):541-547.
14. Franco EB, Benetti AR, Ishikiriama SK, et al. 5-year clinical performance of resin composite versus resin-modified glass ionomer restorative system in non-carious lesions. Oper Dent. 2006;31(4):403-408.
15. Santamaria MP, Suaid FF, Casti MZ, et al. Coronally positioned flap plus resin-modified glass ionomer restoration for the treatment of gingival recession associated with non-carious lesions: A randomized controlled clinical trial. J Periodontol. 2008;79(4):621-628.